Coronary artery disease
Coronary artery disease (CAD) is an affection of the arteries that supply blood to the heart muscle. These arteries are vital and their disease can lead to deterioration of heart function or cardiac arrest.
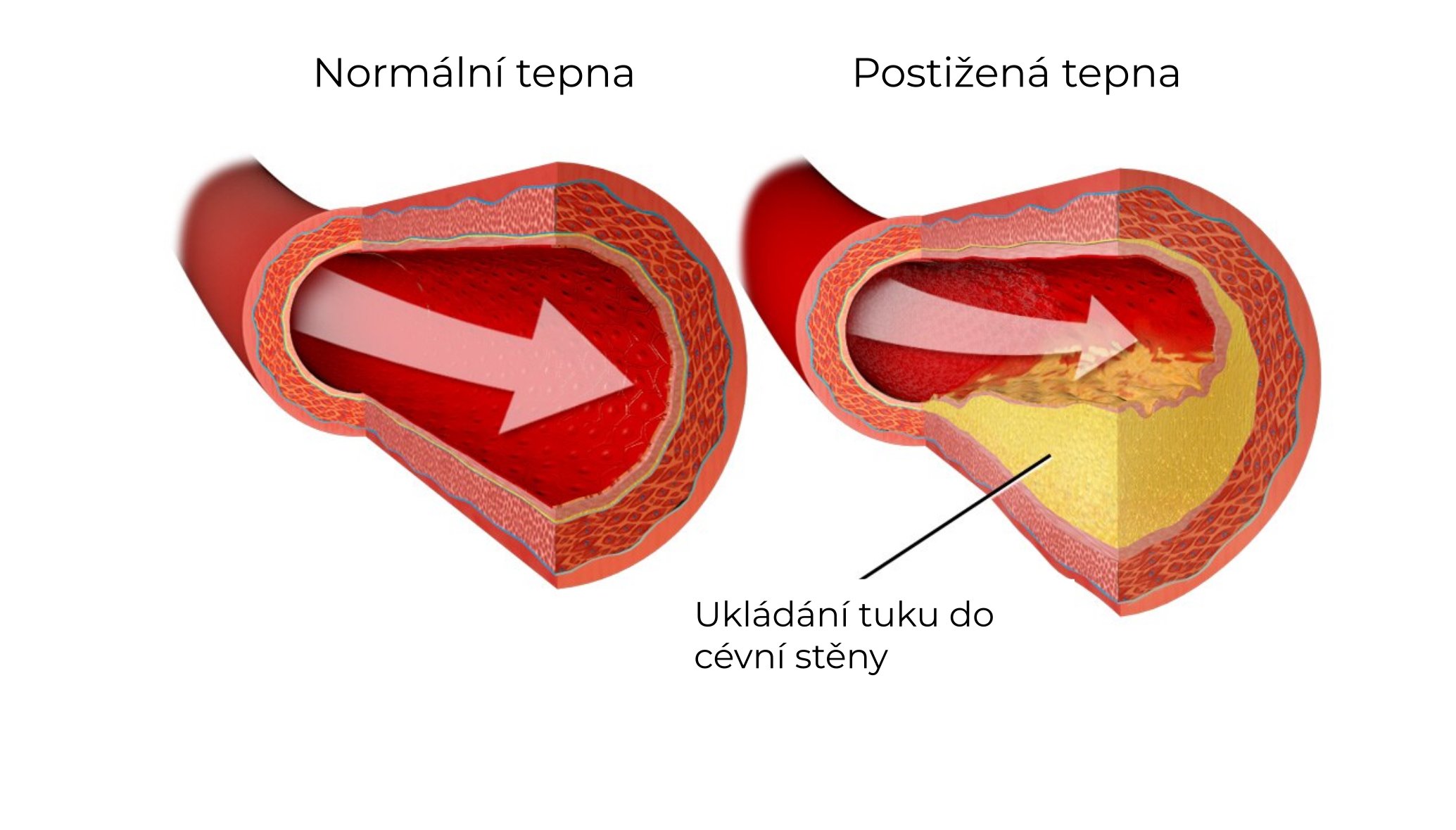
Coronary artery disease is most commonly caused by atherosclerosis, a process in which fatty particles are gradually deposited in the blood vessel wall. The blood vessel responds to the presence of this foreign matter by forming connective tissue and depositing calcium. This results in the formation of an atherosclerotic plaque, which has varying proportions of fat, connective tissue and calcium. The vessel becomes stiffer and the plaque may narrow its internal lumen. If the cover of the plaque ruptures, the masses of the plaque become exposed and the flowing blood forms a clot on them. The clot thus formed can either significantly narrow the vessel or close the vessel completely. Soft plaques with a higher proportion of fat are more prone to rupture. Stiff, fibrous and calcified plaques are less prone to rupture.
Schematic representation of atherosclerosis. The affected artery on the right has a fat-rich atherosclerotic plaque in its wall.
The formation of atherosclerotic plaques is more common in men, in patients with high blood pressure, in smokers, in overweight or obese individuals and in individuals with a sedentary lifestyle. Susceptibility to atherosclerotic plaques is also hereditary and if an individual's parents had Coronary artery disease at an age younger than 50 years, their offspring are likely to be at increased risk of atherosclerosis. A separate and very important risk factor is then diabetes, or diabetes mellitus. Its quality treatment is important in preventing the development of vascular complications. Hereditary forms of elevated cholesterol levels are also associated with an increased risk of developing atherosclerosis and coronary disease. Cholesterol levels are also increased in the presence of the above risk factors such as smoking, overweight, obesity and sedentary lifestyle, and influencing these risk factors can reduce blood cholesterol levels. The overall risk of developing cardiovascular disease can be estimated from the SCORE2 table - the figure indicates what percentage of healthy people will develop the disease in the next 10 years.
Table estimating the risk of developing cardiovascular disease in the next 10 years as a percentage. Source: Czech Society of Cardiology.
Coronary artery disease manifests itself in different ways. It depends on how quickly the narrowing of the coronary artery occurs and how significant the narrowing is. If the coronary arteries are not yet impeded from flowing blood, the individual may not perceive coronary disease in any way. If the flow through the coronary artery slows down or stops, the disease may already be present, and this is when we speak of the so-called coronary syndrome. If this condition arises suddenly, we call it acute coronary syndrome; if the reduction in flow through the coronary artery occurs gradually and slowly, or if the occlusion of the artery has occurred at some time in the past, we call this condition chronic coronary syndrome.
Differences between acute and chronic coronary syndrome. Acute coronary syndrome is an immediate threat to life.
-
Imminent threat to life
The coronary artery is unstable, the atherosclerotic plaque ruptures, a blood clot forms on it
The chest pain is newly developed or newly aggravated and often persists at rest
According to the extent of heart muscle involvement we distinguish:
Unstable angina - the heart muscle is less well blooded but not yet dying
Acute myocardial infarction - impaired blood flow already causes the heart muscle to die
In case of persistent difficulties, it is necessary to restore the flow through the affected vessel as soon as possible
-
No immediate threat to life
Coronary artery involvement is stable and there is no risk of acute occlusion
We also include conditions after a past acute coronary syndrome, when the artery has been treated or the lesion has stabilized
Chest pain may not be present or occur with increased exertion
Revascularisation is suitable for relieving discomfort and improving heart performance
Impaired blood supply to the heart muscle is most often manifested as chest pain. This pain is often in the form of pressure in the middle of the chest or in the back between the shoulder blades or in the upper abdomen. It is often accompanied by shortness of breath and nausea. In stable, long-standing narrowing of the coronary artery, this pain is present only on exertion and subsides again at rest. In suddenly worsening coronary artery narrowing, the pain may re-emerge or worsen and can often be quiescent, resolving within about 20 minutes. If the artery closes completely, a myocardial infarction occurs, the pain is resting, persistent and only subsides after the heart muscle has died more than 12 hours below the onset of pain.
Typical distribution of chest pain with narrowing or occlusion of the coronary arteries.
Coronary artery disease is detected by imaging of the coronary arteries called coronary angiography. The most accurate method is the catheterisation method, where a contrast medium is injected into each coronary artery using a catheter inserted from an artery in the wrist or groin and these are imaged under X-rays. This method is also called selective coronarography (SCG) - because the contrast agent must be injected selectively into the left and then the right coronary arteries. If significant involvement is found, this method can be directly followed up by treatment of the affected area with possible stent placement. The coronary arteries can also be imaged using CT (computed tomography). This method is not as accurate as catheterisation but is safer because it does not require the insertion of a catheter into the coronary arteries and the contrast medium is administered only through a conventional venous cannula.
Selective coronary angiography (SCG) - a contrast agent is injected into the coronary artery spacing using a catheter inserted from an artery in the wrist or groin, and the coronary arteries are imaged with X-rays.
CT coronary angiography - coronary arteries are imaged non-invasively using computed tomography (CT), contrast medium is injected into a common cannula in a peripheral vein
If coronary artery disease is found, the doctor must decide whether it is appropriate to perform what is called revascularisation, or restoring flow through the coronary artery. This is usually only carried out if the artery is narrowed to more than 50% of its diameter. In acute coronary syndromes, revascularisation should be performed as soon as possible. In the case of chronic coronary syndromes, revascularisation is performed in patients with difficulties or in the case of more extensive findings that could endanger the patient in the future.
Revascularization can be performed by catheterization or surgery. The catheterization approach uses tiny balloons that the doctor inflates in the narrowed area of the artery. To prevent the treated site from narrowing again, a so-called stent is placed in the site. The stent is a tiny tube of metal mesh, first inserted in a folded state on a deflated balloon, after the balloon is inflated the stent expands to its full shape and remains in the artery permanently. The stent in the artery is initially bare and there is an increased risk of blood clotting, so two drugs to reduce blood clotting must be taken at the same time - acetylsalicylic acid and, in combination, most often clopidogrel or ticagrelor. Gradually the stent is covered by the vascular lining and the risk of clot formation is reduced. This coverage occurs at different rates and takes at least 1 month. Most stents in use today have a drug on the surface to prevent increased formation of ligament to prevent re-narrowing of the stent site. These so-called 'drug eluting stents' or DES for short are covered by the vascular lining for longer and therefore need to take the aforementioned combination of clot-busting drugs for longer. Collectively, coronary artery catheterization procedures are called percutaneous coronary intervention, or PCI for short.
Schematic representation of percutaneous coronary intervention (PCI) with stent implantation. A thin wire is first inserted into the narrowed coronary artery, followed by a balloon with a folded stent, then the balloon is inflated and the stent is unzipped to keep the vessel patent.
Another way to revascularise the coronary arteries is to surgically sew bridging vessels to guide blood past the narrowed area. These so-called bypasses are sewn by a cardiac surgeon after cutting the sternum to the temporarily stopped heart during extracorporeal circulation. In some cases, the procedure can be performed on a beating heart, where, in addition to the classic approach through the sternum, a less burdensome approach of several smaller incisions in the chest can also be chosen. The artery supplying the pectoral muscle can be used as a bypass. This artery is released and its end is sutured behind the narrowed coronary artery. This type of bypass is very durable and normally works for ten years or more. Another common type of bypass is a venous bypass, where a previously removed superficial vein from the calf is used to bridge the narrowed area. This type of bypass has a shorter lifespan. In addition, an arterial bypass can be used from a previously harvested artery in the forearm. This arterial bypass, like other arterial bypasses, has a longer lifespan. Usually 3-5 bypasses need to be sewn. Surgical revascularization has a greater durability compared to catheterization, but the disadvantage is a greater burden on the body during the procedure. When one coronary artery is affected, catheter revascularization is the preferred choice. In contrast, surgical revascularisation is more common when multiple arteries or the main trunk of the coronary arteries are affected.
Schematic representation of cardiac bypasses - the mammary artery (arteria mammaria) is sutured behind the narrowing on the left coronary artery, the vein taken from the calf is sutured with one end to the aorta and the other end behind the narrowing on the right coronary artery.
If revascularisation has been performed in the past, the treated area may be re-narrowed, so-called restenosis. In addition, patients with known coronary disease also have a higher risk of developing narrowing in previously unaffected coronary artery segments. It is therefore necessary to monitor regularly for chest pain or shortness of breath and to check regularly by echocardiography for worsening left ventricular stiffness.
In patients with coronary artery disease, it is possible to reduce the likelihood of further worsening of the disease by means of regimen and medication. A large effect can be achieved by stopping smoking and getting enough physical activity. Of the drugs, statins have a major effect. Statins are cholesterol-lowering drugs that have been shown to prolong life, reduce the extent of coronary artery disease and reduce the risk of myocardial infarction in patients with coronary artery disease. Another important drug used in coronary disease is acetylsalicylic acid, abbreviated ASA. It blocks the function of platelets and thus prevents the formation of clots on plaques in the coronary arteries. It is taken for life after a myocardial infarction or after a stent has been implanted in the coronary artery. Blood pressure control is also very important. In the case of coronary disease, the recommended blood pressure is no more than 130/80 in the doctor's office. A patient with coronary artery disease should be followed by an outpatient cardiologist who guides treatment, looks for signs of coronary artery disease and motivates the patient to take regimen measures.
A patient with chronic coronary syndrome is regularly checked by an outpatient cardiologist, and it is necessary to take lifelong acetylsalicylic acid and statin therapy. Regimen measures such as sufficient physical activity and avoidance of smoking are important.