Heartbeat
The sensation of palpitations or palpitations is a condition in which the contractions of the heart are clearly perceived by the individual as, for example, skipping, skipping, banging, fluttering or fluttering. Naturally, the contraction of the heart is not felt in any way and therefore palpitations are often unpleasant and the patient may fear for his or her life.
There can be many causes of heart palpitations, and the vast majority of them are not life-threatening. Only in rare cases can it be a side effect of a serious heart condition. In these cases, other complaints such as chest pain, shortness of breath or syncope are often present.
According to the nature of palpitations it is possible to estimate their cause. However, for definitive confirmation, it is necessary to record an ECG when there are difficulties. This can be done either in the doctor's office, or with the help of long-term ECG monitoring called Holter ECG, with the help of attachable ECG recorders or with the help of some smart watches.
A single-lead ECG recorded by a smartwatch can often help identify a possible heart rhythm disorder.
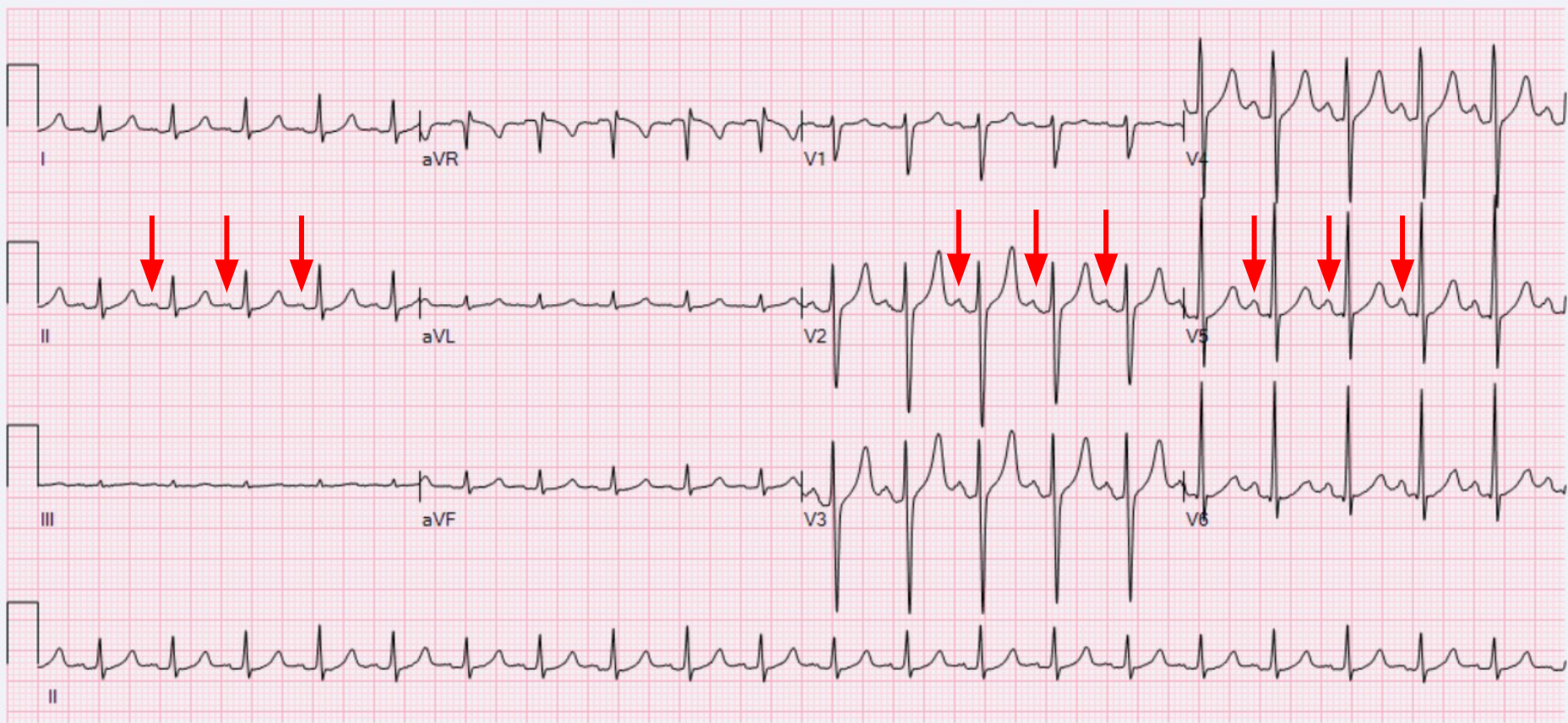
If the palpitations are of the nature of a skipping, skipping or skipping heartbeat and a stronger single thump, these are usually so-called ventricular extrasystoles. This is a condition in which, in contrast to the normal rhythm of contraction of the atria first, followed by the ventricles, the ventricles contract prematurely and empty at a time when they are not yet filled with blood. The blood from the atrial contraction cannot get to the prematurely contracted ventricles and a strange sensation in the throat results. The next normal contraction then occurs after a short pause and is strong because the ventricles are also filled with extra blood from the previous ineffective contraction. This subsequent contraction of the heart is then perceived as a thump. Ventricular extrasystoles can be very uncomfortable for some, others may not perceive them at all. They are often more common in the evening when the basic rhythm of the heart calms down and may then subside on exertion. In a normal healthy heart, ventricular extrasystoles are not threatening and are only treated if they cause significant discomfort. However, the heart should always be carefully examined by a physician to rule out serious disease. Ventricular extrasystoles may disappear completely over time or reappear after some time.
Schematic representation of ventricular extrasystole in the left ventricle. The ECG curve is shown on the right with an arrow indicating ventricular extrasystole.
ECG recording of ventricular extrasystole - shown in red, the heart contraction lasts longer and is followed by a compensatory pause.
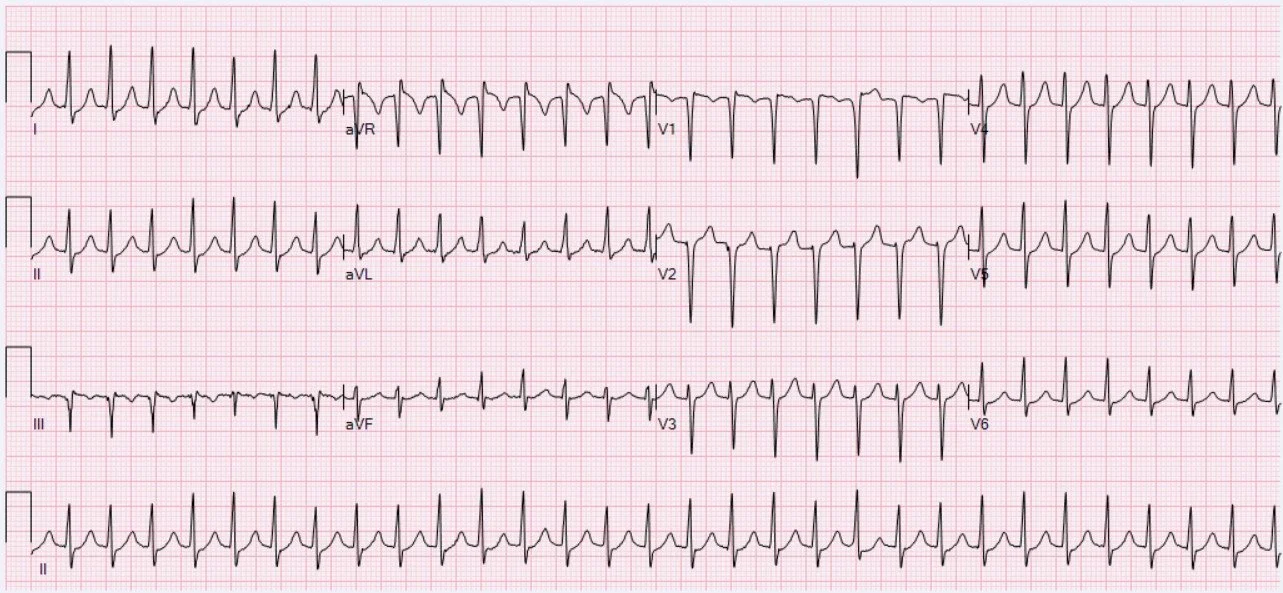
Sometimes the heartbeat may be strong and uncomfortable, but the heart rate may not be significantly faster and may be around 100/min, for example. In these cases, it is often not a heart rhythm disturbance and the cause may lie in the activation of the stress component of the willed nervous system. This is activated, for example, by agitation, anxiety or a feeling of threat. However, activation of the stress nervous system can also occur unexpectedly and without an apparent triggering cause, and thus the individual may, for example, be awakened during the night or the palpitations may occur in another unexpected situation. Again, the heart should be examined in more detail and blood samples should be taken to rule out an increased thyroid function, which may manifest itself in a similar way. It is ideal to record an ECG when there are difficulties, for example with a smartwatch. In these cases, the ECG captures the natural sinus rhythm or its acceleration, the so-called sinus tachycardia.
Sinus tachycardia - a natural, but accelerated rhythm. Arrows indicate contractions of the atria, which precede contractions of ventricles. The heart rate is higher than 100/min in tachycardia.
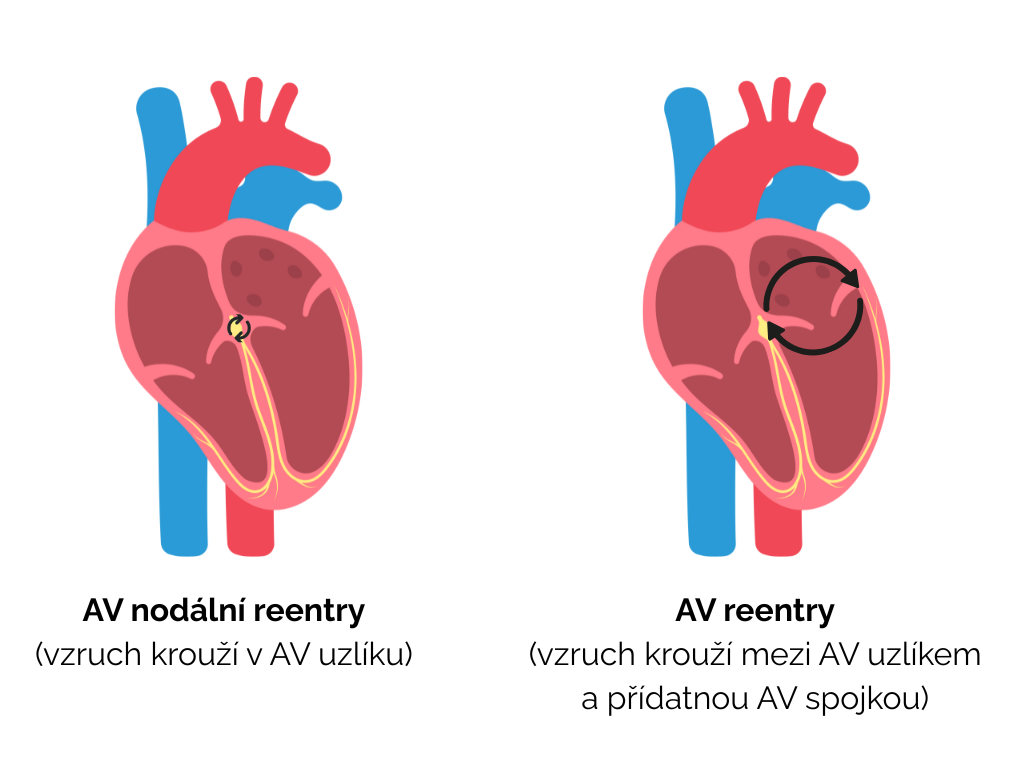
A sudden onset of a very rapid heartbeat with a frequency of around 200/min is most often a heart rhythm disturbance, when the impulse, once transferred from the atrium to the ventricle, is transferred back to the atrium and the impulse becomes stuck - this condition is called "reentry". These rhythm disturbances are in the vast majority of cases non-threatening. They arise and end abruptly and the individual often finds a way to end the palpitations, for example by taking a deep breath or contracting the abdominal muscles. Often there is a concomitant pounding in the throat and sometimes a feeling of weakness. This includes two rhythm disorders - AV nodal reentry tachycardia (AVNRT) a AV reentry tachycardia (AVRT). These rhythm disturbances can be very well treated by catheter removal, or ablation, of the sites where the pacing occurs.
ECG recording of AV nodal reentry tachycardia. Cardiac excitation circles in a nodal pattern between the atria and ventricles, and the atria and ventricles contract simultaneously. Unlike sinus tachycardia, atrial contractions are not apparent on the curve because they are superimposed on the contractions of ventricles.
Schematic representation of two basic rhythm disturbances originating from the AV node. The presence of a pathway that allows the cardiac impulse to loop is always necessary. In the case of AV nodal reentry tachycardia, this pathway is directly in the AV node. In the case of AV reentry tachycardia, this pathway is located outside the AV node and bridges one of the AV valves. Both arrhythmias can be eliminated by catheter ablation of the pathway allowing shunt.
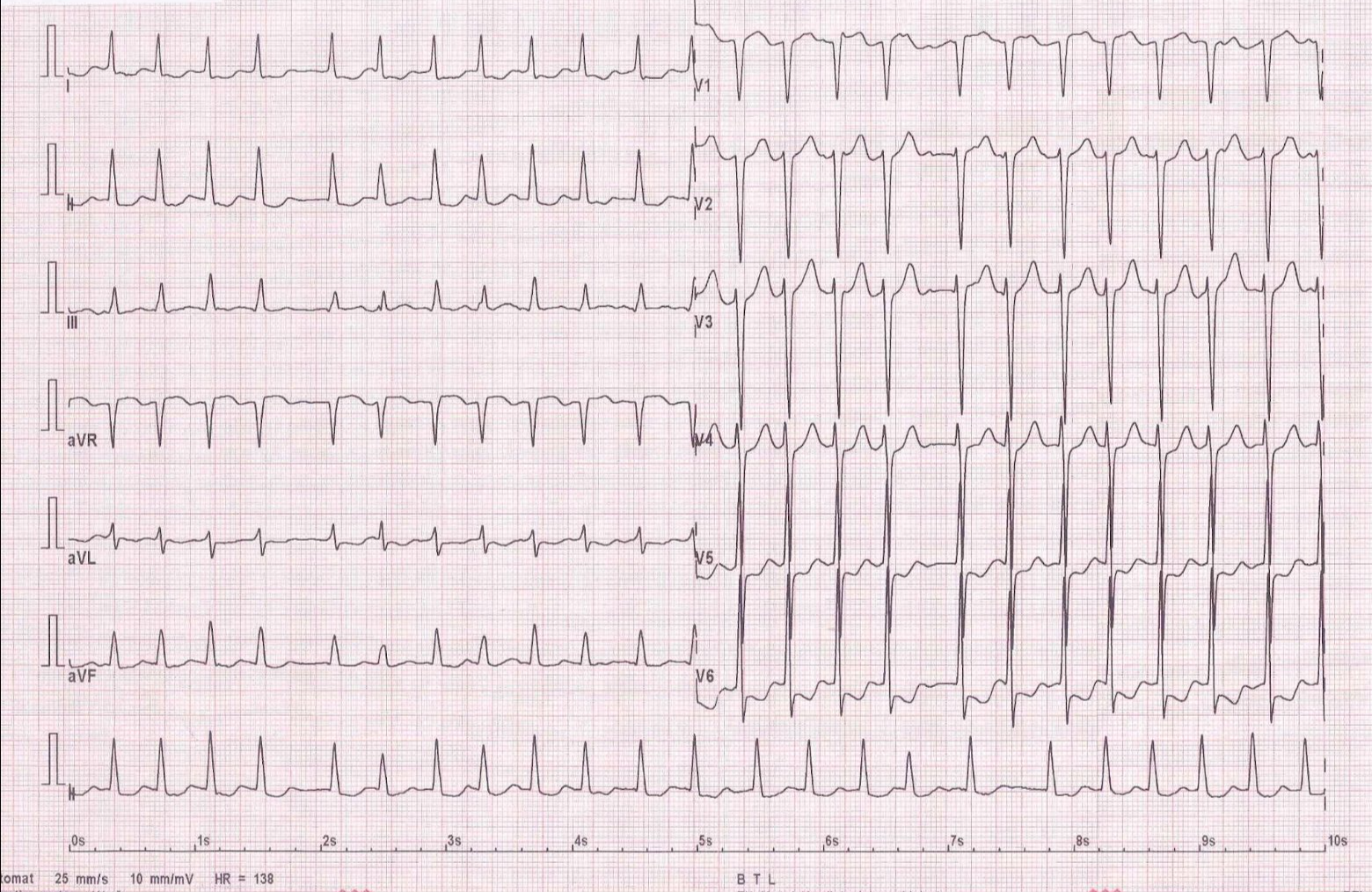
In the case of a rapid but completely irregular heartbeat, this may be the most common heart rhythm disorder, especially in the elderly - atrial fibrillation. The heart seems to flutter and each contraction is perceived differently. At the same time, poorer performance is present. An ECG recording with difficulty establishes the diagnosis. Most smart watches monitor the heart rhythm continuously and warn of possible atrial fibrillation if the rhythm is irregular. When atrial fibrillation is detected, the physician will consider the patient's need for medication to reduce blood clotting and the appropriateness of catheter or drug therapy to prevent recurrence of the arrhythmia.
ECG recording of atrial fibrillation. Atrial contractions are not evident and ventricles contractions are completely irregular.
When a brief, several-second heartbeat occurs, the cause is most often premature contractions or, less commonly, ventricles. These rhythm disturbances, like single extrasystoles, may be transient. If they persist or are accompanied by other complaints such as chest pain or shortness of breath, it is again advisable to examine the heart - record an ECG and perform an echocardiogram.
A fast and regular heartbeat with a frequency of around 130/min. is most often caused by the so-called atrial flutter. In this rhythm disturbance, the electrical excitement in the atria circles around and the atria contract very quickly, at around 260 contractions per minute. Every second atrial contraction is then transmitted to the ventricles, and the ventricles contract at a rate of 130/min. In some parts of the day, every third or every fourth atrial contraction may be converted and the ventricles are contracted at 60-90/min. Otherwise, the rhythm does not fluctuate significantly. If such a fast and stable heart rate is detected by, for example, a smartwatch, an examination by a doctor is advisable. With a prolonged rapid ventricular rate, the function of the ventricles may begin to weaken and the heart may begin to fail. Termination of the rhythm disturbance then leads to full restoration of heart function.
Schematic representation of atrial flutter. On the right side of the figure is an ECG recording with noticeable sawtooth atrial activity, with every fourth atrial contraction transmitted to the ventricle.